In OTC
Follow this topic
Bookmark
Record learning outcomes
One in six people with inflammatory bowel disease (Crohn’s disease or ulcerative colitis) initially receive a diagnosis of irritable bowel syndrome (IBS), and it takes an average of five and a half years to then get a diagnosis of Crohn’s or colitis, according to Crohn’s & Colitis UK. “Crohn’s and colitis affect more than 500,000 people in the UK,” says Ruth Wakeman, director of services, advocacy and evidence at Crohn’s & Colitis UK. “We know that many people are waiting too long for an official diagnosis. The longer you wait to start treatment, the more unwell you can become. It is very important for anyone who is experiencing warning signs, such as blood in poo, stomach pain and frequent, urgent toilet trips, to seek medical advice.”
A new diagnostic pathways website: whatsupwithmygut.org.uk was launched in July 2024. Developed by UK charities, healthcare professional organisations and patients, this website provides support to GPs and other first-contact healthcare professionals to make the process of diagnosing digestive symptoms easier to understand and less overwhelming for patients.
Pharmacy teams are often on the frontline of diagnosis, with customers asking for advice and products. Inflammatory bowel disease (IBD) and irritable bowel disease (IBS) have similar names, share several symptoms, and both flare up and down, so there is often confusion between the two. Yet these are distinct bowel conditions and need very different treatments. It’s important that patients get an accurate diagnosis so that they can manage their symptoms properly and effectively. “IBS and IBD are chronic conditions requiring long-term management,” says Jacquie Lee, medication safety officer and information pharmacist at Numark. “Both conditions can significantly affect a patient’s quality of life, causing discomfort, stress and anxiety.”
What is irritable bowel syndrome?
Irritable bowel syndrome (IBS) affects up to a third of the UK population and is usually diagnosed in people aged 20-40. It’s a functional bowel disorder. The bowel muscles don’t work properly, and the nerves in the gut are more sensitive (‘irritable’) than they should be – leading to uncomfortable symptoms such as abdominal pain, bloating, constipation and diarrhoea. IBS can also cause non-digestive symptoms, such as fatigue and lethargy, nausea, back pain, headaches and an irritable bladder. Research suggests that IBS may be caused by a disturbance between the brain and the gut, changes in the gut microbiota, and/or levels of different hormones or chemicals in the body, such as serotonin. People with IBS are more likely to have other functional disorders, such as fibromyalgia, chronic fatigue syndrome and chronic pelvic pain. Stress can make IBS symptoms worse. Other symptom triggers include certain foods, hormonal changes and some medicines (e.g. non-steroidal anti-inflammatory drugs (NSAIDs)). Unlike inflammatory bowel disease, IBS doesn’t cause inflammation, damage the gut permanently or increase the risk of bowel cancer. However, the symptoms can still be severe and affect day-to-day life.
“Crohn’s and colitis affect more than 500,000 people in the UK”
What is inflammatory bowel disease?
Inflammatory bowel disease (IBD) is an autoimmune condition in which the immune system is overactive. Whereas IBS doesn’t cause any noticeable damage, IBD causes inflammation and ulceration in the lining of the gut, which shows up in diagnostic tests and scans. One in every 123 people in the UK lives with Crohn’s disease or ulcerative colitis (the most common types of IBD), with most people being diagnosed between the ages of 15-40. The tendency to develop IBD often runs in families, but the exact cause is unknown. IBD symptoms include bloating, frequent or urgent diarrhoea (often containing blood), constipation, severe abdominal pain, extreme fatigue and significant weight loss. The exact symptoms vary according to the type of IBD and where the inflammation occurs. Crohn’s disease can affect any part of the digestive tract, but especially the end of the small intestine and beginning of the large intestine (colon). Ulcerative colitis affects only the inner lining of the colon and rectum. Non-digestive symptoms may also occur, such as fevers, joint pain, eye problems and skin problems. Untreated IBD can cause complications such as bowel obstruction and an increased risk of bowel cancer. It can also disrupt school, work, social lives and relationships.
Diagnostic checks
If pharmacy customers have any new or worsening digestive symptoms, it’s important that they speak to their GP. Before confirming a diagnosis of an irritable bowel, doctors will need to rule out other digestive conditions. Initially, their GP may suggest blood tests to check for anaemia, inflammation, infections, coeliac disease and thyroid, kidney or liver problems. They may also suggest doing a stool (poo) test to check for blood, inflammation and infections. Woman aged 50 or over with new IBS symptoms in the previous 12 months should be tested for ovarian cancer. If all of the tests are negative and the symptoms are characteristic of an irritable bowel, patients will probably be diagnosed with IBS and given advice on how to manage their symptoms. However, it’s important that they go back to their GP if their symptoms aren’t getting any better, or if they’re getting worse.
If a GP suspects a patient has IBD from their test results and/or symptoms (such as passing blood), they will be referred to a specialist gastroenterologist for a colonoscopy, biopsy and other investigations (such as a CT scan or MRI). This is also important to rule out bowel cancer. “The earlier bowel cancer is spotted, the more treatable it’s likely to be,” says Claire Coughlan, consultant colorectal nurse and clinical lead for Bowel Cancer UK. “That’s why our new campaign ‘Tell Your GP Instead’ is encouraging people to go to their GP as soon as they spot symptoms. These may include a change in bowel habits, bleeding from the back passage or blood in stools, a pain or lump in the abdomen or rectum, unintentional weight loss, and fatigue. Pharmacy teams are at the forefront of healthcare and often the first port of call if someone has health worries.”
Women aged 50 and over with new IBS symptoms within the last 12 months should be checked for ovarian cancer.
Fibre balance
Adults should ideally have around 30g of dietary fibre each day for good health, but research shows that most adults only consume around 18g. Fibre is essential to ensure the digestive system is working properly. A regular fibre intake increases good bacteria in the gut, which can boost the immune system and dampen down inflammation, and reduces the risk of chronic diseases such as cardiovascular disease, type 2 diabetes and bowel cancer.
Soluble fibre (soft and moist – in fruit and oats, for example) attracts water to stools and is good for constipation. Insoluble fibre (tougher and harder to digest – found in wheat bran and nuts, for example) adds bulk to stools. Resistant starch (found in oats, wheat bran, nuts and lentils, for example) isn’t digested by the small intestine, but acts as food (prebiotic) for gut bacteria. To increase fibre intake, swap white flour, bread, rice and pasta for wholemeal and wholegrain versions, and have five portions of fruit and vegetables a day. Add fruit, nuts and seeds into breakfast cereal or yoghurt, include extra vegetables or beans to bolognese, curry and chilli, or dip apple slices, carrot sticks or celery into chunky nut butters or hummus as a snack. If someone wants to increase their fibre intake, they should do this slowly – to make sure it doesn’t affect their bowels. It’s also important to drink plenty of fluid, as fibre draws water into the bowel, increasing the risk of dehydration.
“The earlier bowel cancer is spotted, the more treatable it’s likely to be”
Managing IBS
Irritable bowel syndrome can usually be managed with medicines, dietary changes, trigger awareness and stress relief. There’s no one-size-fits-all solution, and it often takes trial and error to find the best approach. “Self-help advice can include eating small, regular meals every four to five hours and trying not to skip meals,” says Jacquie. “It may also help to avoid large meals and rich/fatty foods late at night. When eating, do so slowly, chewing food properly, and drink sufficient fluids throughout the day (limiting caffeinated, fizzy and alcoholic drinks). Ensure adequate daily fibre intake and reduce the amount of fat in the diet. Quit smoking, take regular exercise and manage stress.” Many of the medicines for IBS are available over the pharmacy counter, although stronger medicines can be prescribed by a GP. Typical pharmacy medicines for IBS include laxatives, anti-diarrhoeals, peppermint capsules and antispasmodics (which stop the bowel muscles from contracting). “IBS treatment depends on the person’s symptoms,” says Julie Thompson, information manager at Guts UK. “For people with IBS and reflux symptoms, peppermint might make reflux symptoms worse. Laxatives may help constipation-based IBS symptoms, although avoid lactulose, which is a fermentable sugar. Tricyclic antidepressants could be prescribed as a second-line treatment if other medicines haven’t helped. At low doses, amitriptyline acts directly on the gut to reduce IBS symptoms.” Stress, anxiety and depression can make IBS worse, so seeing a counsellor or trying mindfulness or relaxation therapies may help. “Referral for psychological interventions can be considered for people with IBS by their GP if they haven’t responded to medication after 12 months if symptoms continue,” says Julie. “Examples are cognitive behavioural therapy (CBT), gut-directed hypnotherapy and/or psychological therapy.”
Stool health
Everyone’s stools (poo) varies in colour and consistency. Guts UK have developed a helpful way to monitor poo health at: gutscharity.org.uk/poo-torial/
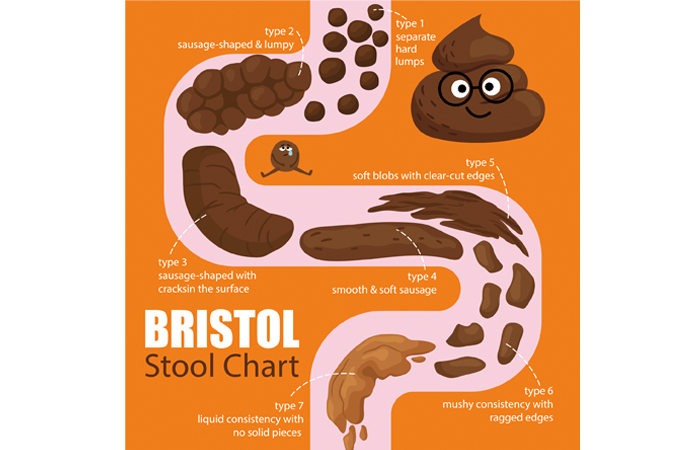
Also available is the Bristol Stool Chart, a medical aid that classifies stools into seven different types:
Type 1: Separate hard lumps, like nuts (hard to pass)
Type 2: Sausage-shaped but lumpy
Type 3: Like a sausage but with cracks on the surface
Type 4: Like a sausage or snake, smooth and soft
Type 5: Soft blobs with clear-cut edges
Type 6: Fluffy pieces with ragged edges, a mushy poo
Type 7: Watery, no solid pieces. Entirely liquid
A normal stool is considered to be types 3 or 4. Types 1 and 2 usually indicate constipation, while types 5 to 7 are varying stages of diarrhoea.
IBD management
Inflammatory bowel disease treatment usually involves taking prescribed medicines to reduce inflammation in the bowel, although mild symptoms may respond to lifestyle changes. Prescribed medicines include aminosalicylates (which reduce inflammation), immunosuppressants (which dampen down the immune response), corticosteroids (taken short-term during a flare-up) and biologic medicines for more severe symptoms. Up to 80 per cent of people with Crohn’s disease, and 15 per cent of those with ulcerative colitis, will need to have surgery at some point in their lives. “Most people living with inflammatory bowel disease take regular prescription medication to control their symptoms,” says Ruth. “For many, they will receive their medicine directly from the hospital, but some people with IBD will also be prescribed medicines by their GP. That means they’re likely to visit the pharmacy regularly. Having a good relationship with a knowledgeable pharmacy team will help them feel supported as they navigate the challenges of dealing with a lifelong condition.” People with inflammatory bowel disease need to be careful about taking some pharmacy medicines, such as NSAIDS. They should also speak to their GP before taking over-the-counter (OTC) medicines for diarrhoea, constipation or stomach cramps, as these may worsen their symptoms. “Any signs of a flare-up not responding to management strategies indicates that the customer needs to be referred to a GP,” says Jacquie. “If the patient experiences side effects from their medications or requires advice on prescription adjustments, this too is an issue the GP needs to be made aware of. It is strongly advised that patients with Crohn’s disease quit smoking, and community pharmacy teams can encourage stress management techniques, as stress can worsen symptoms.”
“Up to 80 per cent of people with Crohn’s disease will need to have surgery at some point in their lives”
Dietary changes
Many people with IBS or IBD notice that what they eat and drink affects their symptoms. There’s no single eating plan that works for everyone, but it can help to keep a diary to see if certain food groups or eating habits make the symptoms better or worse. Speaking to a dietitian is important to help patients learn which foods to eat and avoid, while making sure they are still getting the essential nutrients.
Common dietary triggers of bowel symptoms include dairy products (lactose), gassy foods (such as beans, cabbage and broccoli), spicy foods, alcohol, caffeine and chocolate. While a high fibre diet can help constipation, other people can’t tolerate large amounts of fibre, experiencing bloating, gas and diarrhoea. Limiting or avoiding FODMAPs, a type of sugar particularly high in certain fruits and vegetables, legumes and pulses, wheat and other grains, and some dairy products, may help certain people with IBS. Some people with IBD may need a special liquid diet to control their symptoms, under the guidance of a doctor or dietitian. “Don’t advise people [to] follow a single exclusion diet or elimination diet (for example, lactose free, low FODMAP or gluten free),” says Jane. “Recommend they see their GP. If the person wishes to trial a diet to see what they are intolerant too, they should be referred to a registered dietitian so that eating disorders are screened for and the treatment can be administered safely.”